 |
.
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . .

The
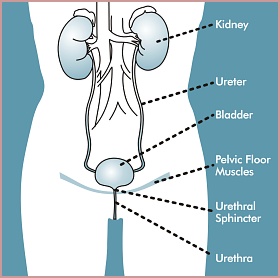
urinary system consists of the kidneys, ureters, bladder, urethra,
and the pelvic floor muscles.
 The
kidneys
function as a filter to remove waste products from the blood
stream. These waste products (urine) are moved through the
ureters for storage in the bladder. The
bladder is composed of smooth muscles that relax during bladder filling.
The relaxed muscles help the bladder expand like a balloon to accommodate the storage of
urine. Urination begins when these muscles
contract forcing the urine out
of the bladder. The
urethra, which extends from
the base of the
bladder, is a hollow muscular tube that allows emptying of
the bladder. At
the connection of the urethra to the bladder is a group of circular muscles called sphincters, which act as a valve that
controls the flow
of urine. This
urethral sphincter contracts (the valve is closed)
during bladder filling and storage, and relaxes (the valve is
opened) during emptying. The
kidneys
function as a filter to remove waste products from the blood
stream. These waste products (urine) are moved through the
ureters for storage in the bladder. The
bladder is composed of smooth muscles that relax during bladder filling.
The relaxed muscles help the bladder expand like a balloon to accommodate the storage of
urine. Urination begins when these muscles
contract forcing the urine out
of the bladder. The
urethra, which extends from
the base of the
bladder, is a hollow muscular tube that allows emptying of
the bladder. At
the connection of the urethra to the bladder is a group of circular muscles called sphincters, which act as a valve that
controls the flow
of urine. This
urethral sphincter contracts (the valve is closed)
during bladder filling and storage, and relaxes (the valve is
opened) during emptying.
The brain and spinal cord regulate this complex system, and a
malfunction in any part of this system can lead to incontinence.
.
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . .

Stress
Incontinence
Stress Incontinence is a bladder storage defect. The bladder is
unable to store urine until voluntary urination occurs. This is
either due to pelvic support problems, such as weak surrounding
muscle, a urethral sphincter defect, or both. The
pelvic muscles that ordinarily force the urethra closed do not
squeeze as tightly as they should. Urine is lost when
the patient laughs, coughs, sneezes, or performs any physical
activity that increases the abdominal pressure to a level which
overcomes the bladder's retention capability. Stress Incontinence
is the most common form of urinary incontinence, accounting for
approximately 40% of all cases. It is most common among women
under 60. Treatments for
Stress Incontinence focus on toning pelvic neuromuscular tissue.
Urge
Incontinence
Urge
Incontinence, or Detrusor Instability, is a bladder filling defect. Involuntary muscle
contractions cause a loss of urine. A common symptom is a strong
and frequent desire
to urinate. Normally, bladder muscles allow slow filling by
expanding. As the bladder fills, nerves are stimulated
to send messages to the brain.
For those with urge incontinence, the bladder may
inappropriately contract at any time during filling. This occurs
when the nerve and muscle systems from the bladder to the brain
are damaged or malfunctioning. Patients may describe a sudden urge
to urinate and an involuntary loss of urine associated with
touching or hearing running water, touching their doorknob when
entering their home, drinking a small amount of liquid, or during sleep. Urge Incontinence accounts
for about 30% of all cases and is more common among older adults.
Treatments for Urge Incontinence work on calming the involuntary
bladder muscle contractions and retraining the bladder function.
Mixed
Incontinence
Mixed
Incontinence is a combination of stress and urge incontinence and
accounts for about 30% of all cases. Older women are most likely
to experience this combination incontinence.
.
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . .

The U.S.
Department of Health and Human Services' Agency for Health Care
Policy and Research has established clinically accepted standards
for the diagnosis and treatment of urinary incontinence. These
standards, developed by an expert panel of doctors, nurses and
other health care specialists,
recommend the least invasive
treatments as the first choice for sufferers of incontinence.
Behavioral Therapies (least invasive)
 Pelvic Muscle Exercises or Kegel Exercises can substantially
improve, and even prevent, urinary incontinence. Properly
performed Kegel exercises increase the strength of weakened pelvic
floor muscles, reducing or stopping involuntary leaks associated
with Stress Incontinence, and improving control over the urgency
brought on by involuntary bladder contractions associated with
Urge Incontinence.
Pelvic Muscle Exercises or Kegel Exercises can substantially
improve, and even prevent, urinary incontinence. Properly
performed Kegel exercises increase the strength of weakened pelvic
floor muscles, reducing or stopping involuntary leaks associated
with Stress Incontinence, and improving control over the urgency
brought on by involuntary bladder contractions associated with
Urge Incontinence.
 Pelvic
Floor Stimulation (PFS)
uses a special electrical signal, or waveform, that automates Kegel
exercises. One electrical waveform exercises and strengthens the muscles
of the pelvic floor to treat Stress Incontinence. A different electrical
signal is used to treat Urge Incontinence. This signal works to calm
involuntary bladder muscle contractions. Mixed Incontinence is treated
by alternating the two electrical signals in a special treatment schedule.
Pelvic
Floor Stimulation
has clear advantages over Kegel
Pelvic
Floor Stimulation (PFS)
uses a special electrical signal, or waveform, that automates Kegel
exercises. One electrical waveform exercises and strengthens the muscles
of the pelvic floor to treat Stress Incontinence. A different electrical
signal is used to treat Urge Incontinence. This signal works to calm
involuntary bladder muscle contractions. Mixed Incontinence is treated
by alternating the two electrical signals in a special treatment schedule.
Pelvic
Floor Stimulation
has clear advantages over Kegel exercises because it always exercises the correct muscles, permits
treatment of patients without enough muscle strength to correctly
perform the exercises, and does not require active concentration on
what can be a very demanding exercise schedule. Clinical research
studies report greater than 70% "significant improvement"
rates for Stress, Urge and Mixed Incontinence using PFS.
exercises because it always exercises the correct muscles, permits
treatment of patients without enough muscle strength to correctly
perform the exercises, and does not require active concentration on
what can be a very demanding exercise schedule. Clinical research
studies report greater than 70% "significant improvement"
rates for Stress, Urge and Mixed Incontinence using PFS.
 Biofeedback is
a monitoring tool to measure pelvic muscle activity, which helps
increase patient awareness and control of pelvic muscle contractions when
performing Kegel exercises. A clinician may also use biofeedback
to measure the success of PFS therapy.
Biofeedback is
a monitoring tool to measure pelvic muscle activity, which helps
increase patient awareness and control of pelvic muscle contractions when
performing Kegel exercises. A clinician may also use biofeedback
to measure the success of PFS therapy.
 Vaginal Weight Training is a method for strengthening the pelvic
muscles by holding a series of progressively heavier
specially-shaped
weights within the vagina when tightening the pelvic muscles.
Vaginal weights are only used
in the treatment of Stress Incontinence.
Vaginal Weight Training is a method for strengthening the pelvic
muscles by holding a series of progressively heavier
specially-shaped
weights within the vagina when tightening the pelvic muscles.
Vaginal weights are only used
in the treatment of Stress Incontinence.
 Bladder Training is a group of techniques that instruct an
individual to resist the urge to urinate and gradually expand the
time intervals between urination. These techniques are helpful in
the treatment of Urge Incontinence.
Bladder Training is a group of techniques that instruct an
individual to resist the urge to urinate and gradually expand the
time intervals between urination. These techniques are helpful in
the treatment of Urge Incontinence.
Drug Therapies (more invasive, with possible side effects)
 Oxybutynin
and Tolterodine Tartrate relax the
bladder muscles to help reduce the spasms associated with Urge Incontinence.
Oxybutynin
and Tolterodine Tartrate relax the
bladder muscles to help reduce the spasms associated with Urge Incontinence.
 Estrogen, taken orally or vaginally, may be helpful in treating
postmenopausal women. Estrogen may be effective only when used along with other treatments.
Estrogen, taken orally or vaginally, may be helpful in treating
postmenopausal women. Estrogen may be effective only when used along with other treatments.
Surgical Therapies
(most invasive)
 Sling Procedures are surgical procedures
that use natural tissue or artificial material to create a sling
that supports the
bladder. The ends of the sling are
attached to the pubic bone or attached to the abdomen above the
pubic bone. Sling procedures can cure stress incontinence for 4 years in 80 percent
of cases, but do often require repeat surgeries. These procedures
have a moderate risk of infection.
Sling Procedures are surgical procedures
that use natural tissue or artificial material to create a sling
that supports the
bladder. The ends of the sling are
attached to the pubic bone or attached to the abdomen above the
pubic bone. Sling procedures can cure stress incontinence for 4 years in 80 percent
of cases, but do often require repeat surgeries. These procedures
have a moderate risk of infection.
 Bulking Injections. A bulking agent like Collagen is injected into
the tissue surrounding the bladder neck and urethra to add bulk
and help close the bladder opening. Repeat injections are often
necessary, since the body works to eliminate the Collagen. This technique is used to reduce Stress
Incontinence.
Bulking Injections. A bulking agent like Collagen is injected into
the tissue surrounding the bladder neck and urethra to add bulk
and help close the bladder opening. Repeat injections are often
necessary, since the body works to eliminate the Collagen. This technique is used to reduce Stress
Incontinence.
|

